If you’re knee-deep in patient charts or juggling endless appointments, you’ve probably heard the buzz about artificial intelligence in the healthcare sector. It’s popping up everywhere, from diagnostic tools to administrative helpers. AI in healthcare is already reshaping things, like spotting patterns in scans that might slip past tired eyes. Of course, it’s not all sunshine; there are hurdles to clear.
This blog takes you on a closer look at the promises, potential drawbacks, and thought-provoking ethical puzzles that come with weaving AI into everyday medical practice.
How is AI in Healthcare a Game-Changer for Busy Professionals?
Artificial intelligence in healthcare brings a ton of promise to the table, making processes faster and more precise. Doctors and nurses are swamped these days, and AI steps in like a reliable sidekick.
For instance, tools powered by this tech can sift through mountains of data in seconds, something that would take humans hours. But before we get too excited, it’s worth pondering whether AI should be used in healthcare in every scenario. Not every tool is ready for prime time, yet the potential is enormous.
10 Benefits of Artificial Intelligence in Healthcare
This tech isn’t just hype; it’s delivering real results in clinics and hospitals. AI helps deliver crisper diagnoses, use resources more wisely, boost efficiency, support medical staff, and improve patient outcomes.
Below are some standout ways this technology is reshaping care and transforming everyday practice.
1. Enhanced Diagnostic Accuracy
One standout is how it sharpens diagnoses. Machines can analyze images like X-rays or MRIs with pinpoint precision, catching issues early.
A study from Harvard Medical School points out that AI spots fractures or tumors that humans might miss, leading to quicker treatments and better survival rates. CHIEF, a cutting-edge AI for pathology, trained on millions of tissue images, analyzes slides comprehensively and beats other models by up to 36% in detecting cancer, identifying tumors, predicting outcomes, and analyzing genes across diverse global datasets.
2. Predictive Analytics for Prevention
AI excels at forecasting risks, like predicting disease outbreaks or patient readmissions. Tools scan patterns in population data to flag potential problems, helping providers intervene before things escalate.
3. Accelerated Drug Discovery
In research labs, AI sifts through compounds at lightning speed to find promising drugs. This slashes development time and costs, bringing new therapies to market faster. Imagine the impact on chronic conditions like cancer or diabetes.

4. Improved Patient Monitoring
Wearables and sensors powered by AI track vital signs in real time, alerting teams to changes. This is huge for remote care, especially in rural areas where access is limited.
5. Personalized Treatment Plans
Another gem is crafting personalized treatments that fit each patient like a glove. By crunching genetic data and health histories, AI suggests options that match individual needs. This means fewer trial-and-error approaches and more effective care right from the start.
BMC Medical Education notes that AI is now widely applied in healthcare for diagnostics and tailored treatment plans, highlighting the need for its responsible and beneficial development.
6. Reduced Staff Burnout
By automating routine jobs, AI lets professionals focus on complex cases. These boost job satisfaction and lower turnover, a win for everyone in the field.
7. Cost Savings Across the Board
Hospitals save big by optimizing resources, from inventory to staffing. AI predicts demand, cutting waste and trimming budgets without skimping on quality.
8. Streamlined Administrative Tasks
Nobody loves paperwork, right? AI handles scheduling, billing, and record-keeping, freeing up staff for what matters most: patients. This cuts down on errors and speeds up operations, making the whole system run like a well-oiled machine.
According to the American Medical Association, most physicians view AI as especially useful for handling documentation tasks such as billing codes, visit notes, discharge instructions, and patient messages, while also seeing value in areas like prior authorization, translation, chart summaries, and research updates.
9. Enhanced Telemedicine Services
Finally, AI boosts virtual visits with chatbots for triage and automated follow-ups, expanding access to care for underserved groups.
10. Better Clinical Trial Design
AI refines trials by selecting ideal participants and monitoring progress, making studies more efficient and reliable. AI voice assistants are now used in many clinical trials. They remind patients about appointments, track their daily activities, help sites and sponsors stay connected, and keep doctors more informed, as per PMC.
Advantages and Disadvantages of Artificial Intelligence in Healthcare
Now, let’s examine the opportunities and challenges of artificial intelligence in healthcare.
Advantages
- Speeds up decision-making, especially during emergencies, by providing instant data insights.
- Democratizes care, giving patients access to high-level expertise through apps and smart devices.
- Reduces human errors in medical practices, creating safer environments for patients and staff.
Disadvantages
- High setup costs can make adoption difficult for smaller clinics.
- Risk of over-reliance on systems; glitches could lead to mistakes.
- Poor data quality can harm results; bad inputs produce bad outputs.
- Job shifts may occur as some roles change or disappear.
- Ethical dilemmas remain, including accountability when AI makes errors.
If planning to scale your setup, talking with healthcare practice brokers, like Strategic Medical Brokers, can help with expansions or partnerships.
Ethical Concerns of AI in Healthcare
Diving into the ethical concerns of AI in healthcare, things get thorny. Privacy tops the list; with so much sensitive data involved, leaks could devastate trust. Bias in algorithms is another red flag, potentially worsening disparities if training data skews toward specific groups. A CDC report warns that unchecked AI might amplify health inequities.
Accountability is tricky, too. Who owns up if an AI suggestion harms a patient? Informed consent matters; patients should know when tech influences their care. The World Health Organization calls for safeguards to prevent errors that erode confidence. These ethical concerns of AI in healthcare demand clear guidelines and ongoing oversight to ensure fairness.
In healthcare, transparency is vital. Systems should explain decisions in plain terms, not black-box mysteries. Liability questions linger; courts might need to redefine responsibility.
According to IBM, more than half of healthcare executives, 53%, say that cybersecurity and patient data protection are their most significant challenges. And 54% are concerned that they do not currently have the right internal clinical capabilities to deliver, deploy, and scale AI systems.
Bioethics frameworks highlight key areas such as patient safety, data protection, informed consent, and responsibility. The chart below, from PMC, illustrates which of these principles are most often discussed in relation to AI in healthcare.
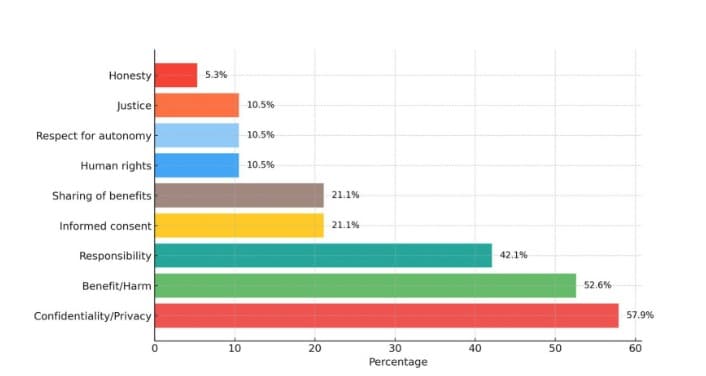
Chart Source: PMC
The chart shows that, in AI for medicine, protecting privacy and ensuring patient safety are seen as the most critical ethical priorities, while aspects like honesty and justice receive less focus.
FAQs
AI processes scans and tests rapidly, highlighting anomalies for quicker reviews by doctors.
No, it supports them by handling data-heavy tasks, but human empathy and judgment remain essential.
It analyzes speech or text for mood patterns, aiding therapists in early interventions.
Strong encryption and regulations help, but ongoing vigilance is needed to prevent breaches.
Robotic assistants guided by AI are becoming common, offering precision in complex operations.
Final Words
AI in healthcare holds massive potential to transform the medical field for the better. While debates continue, the evidence leans toward thoughtful integration. It enhances efficiency, personalizes care, and tackles tough challenges, but we must address downsides head-on. As professionals, staying informed and adaptable is crucial.
If you’re eyeing growth, consider tools for medical practice valuation to gauge your setup’s worth in this evolving landscape. Ready to optimize your practice? Reach out to Strategic Medical Brokers today for expert guidance on buying, selling, or valuing your medical business and chat about your goals.